


Versión Traducida
BACKGROUND
A 57-year-old man presents to a local emergency department with severe abdominal
pain after being evacuated from a cruise ship. The pain, which is most severe in
the right lower portion of his abdomen, started soon after he boarded the ship 2
days ago. Since then, the pain has worsened, and the patient has noticed his
abdomen becoming progressively "bloated." The pain is associated with
nausea and vomiting. He has not been able to have a bowel movement. On further
questioning, the patient reports having night sweats, low-grade fevers,
intermittent abdominal discomfort with constipation, and a 30-lb weight loss
over the last 2-3 months. He has no significant medical history and is not
taking any medications. He does have a significant family history of colon
cancer, soft tissue sarcoma, pancreatic cancer, chronic myeloid leukemia (CML),
and prostate cancer.
On physical examination, the patient is alert and oriented. His temperature is
98.8°F, his pulse is 65 beats per minute, his respiratory rate is 18 breaths
per minute, and his blood pressure is 104/67 mm Hg. Abdominal examination
reveals localized tenderness to palpation in the right lower quadrant (RLQ),
with a palpable mass. He has generalized abdominal distension but no guarding,
rebound, or percussion tenderness. Rectal examination reveals guaiac-positive,
brown stool. Findings from the respiratory and neurologic portions of the
physical examination are unremarkable.
Laboratory investigations are ordered and reveal a hemoglobin value of 9.4 g/dL,
with a corresponding hematocrit of 30.8%. His WBC count is 6.2 X 109/L,
and his lactate dehydrogenase (LDH) level is elevated at 285 U/L. Results of an
electrolyte panel, liver function tests, and renal function tests are within
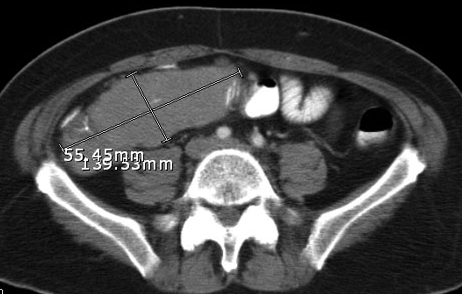
normal limits. Abdominal CT is performed, which demonstrates a large right lower
quadrant mass (see Image). The mass causes a small-bowel obstruction, and
several enlarged retroperitoneal and mesenteric nodes are noted (not pictured).
What is the likely etiology of this mass, and what is its treatment?
Answer
Diffuse, large B-cell lymphoma (DLBCL): Needle biopsy of the RLQ mass revealed a DLBCL involving the intestinal wall. Bone marrow aspiration revealed normocellular marrow negative for lymphoma. After diagnosis, the patient received a round of CHOP chemotherapy, which consists of vincristine, doxorubicin, prednisone, and cyclophosphamide (nitrogen mustard), along with dexamethasone (Decadron) and granulocyte colony-stimulating factor (G-CSF).
Prophylactic surgery to remove the RLQ mass was scheduled because of the relatively high risk of ileocecal bowel perforation during and after chemotherapy because of the lymphoma's extensive infiltration of the entire bowel wall, as seen on CT. The preoperative diagnosis was non-Hodgkin lymphoma (NHL), ie, DLBCL of the small bowel. After surgery, lymphoma to the terminal ileum, right colon, and mesentery of the small bowel were confirmed. The terminal ileum and proximal right colon were resected, and an ileocolic anastomosis was made.
Lymphomas are categorized as Hodgkin lymphoma or NHL. Hodgkin lymphomas are most often localized to a single axial group of nodes, they spread contiguously, and they rarely cause extranodal involvement. In contrast, NHL most frequently involves several peripheral nodes, they have noncontiguous or disseminated spread, and they commonly result in extranodal involvement. NHL can be further categorized into B-cell and T-cell lymphomas. DLBCL is a malignancy of mature B-cells originating from the germinal center or marginal-zone B cells. It is the most common histologic subtype of B-cell NHL, accounting for 20% of all NHLs and 60-70% of aggressive lymphoid neoplasms. On histologic evaluation, DLBCL-involved lymph nodes show a diffuse pattern of involvement with loss of normal structures, such as sinuses and lymphoid follicles.
The median age when DLBCL occurs is in the 60s, and the patient often presents with a rapidly enlarging, symptomatic mass, typically in the neck or abdomen. As many as 40% of patients present with extranodal involvement. The ileum is the most common site of extranodal lymphoma, which accounts for 5% of all lymphomas. As in this case, mass effect can lead to small SBO. Depending on the extranodal location of the lymphoma, other presentations due to mass effect include superior vena cava (SVC) syndrome, tracheobronchial compression leading to respiratory distress, and spinal-cord compression related to destruction of bone in the vertebral column. Detection of tumor in the bone marrow is associated with spread to the CNS in 10-20% of patients.
Constitutional symptoms include fever, weight loss, and drenching night sweats and occur in 30% of patients. More than 50% have elevated serum LDH levels. The International Non-Hodgkin's Lymphoma Prognostic Factors Project reports a 5-year survival rate of 26-73%; the exact rate depends on the number of risk factors and the histologic type. Risk factors for increased mortality and relapse include age older than 60 years, increased serum LDH level, Ann Arbor stage III or IV, and more than 1 extranodal disease site. The mean long-term disease-free survival rate is about 40%. Relapse is most common in the first 2-3 years after diagnosis, with relapse relatively uncommon after 4 years.
For more information on DLBCL, see the eMedicine articles Lymphoma, B-Cell and Lymphoma, Diffuse Large Cell (within the Internal Medicine specialty).
References
Freeman HJ. Free perforation due to intestinal lymphoma in biopsy-defined or suspected celiac disease. J Clin Gastroenterol 2003 Oct;37(4):299-302.
Gajra A. Lymphoma, B-Cell. eMedicine Journal [serial online]. November 3, 2005. Available at: http://www.emedicine.com/med/topic1358.htm.
Law M, Williams S, Wong J. Role of surgery in the management of primary lymphoma of the gastrointestinal tract. J Surg Oncol 1996;61:199-204.
Randall J, Obeid ML, Blackledge GR. Haemorrhage and perforation of gastrointestinal neoplasms during chemotherapy. Ann R Coll Surg Engl 1986 Sep;68(5):286-9.
ReMine SG, Braasch JW. Gastric and small bowel lymphoma. Surg Clin North Am 1986 Aug;66(4):713-22.
Sakakura C, Hagiwara A, Nakanishis M, et al. Bowel perforation during chemotherapy for non-Hodgkin's lymphoma. Hepatogastroenterology 1999 Nov-Dec;46(30):3175-7.
Wada M, Onda M, Tokunaga A, et al. Spontaneous gastrointestinal perforation in patients with lymphoma receiving chemotherapy and steroids. J Nippon Med Sch 1999;66(1):37-40.